Lupus Research Alliance Awards 2022 Lupus Insight Prize to Immunologist Dr. Akiko Iwasaki: Renowned immunology expert honored
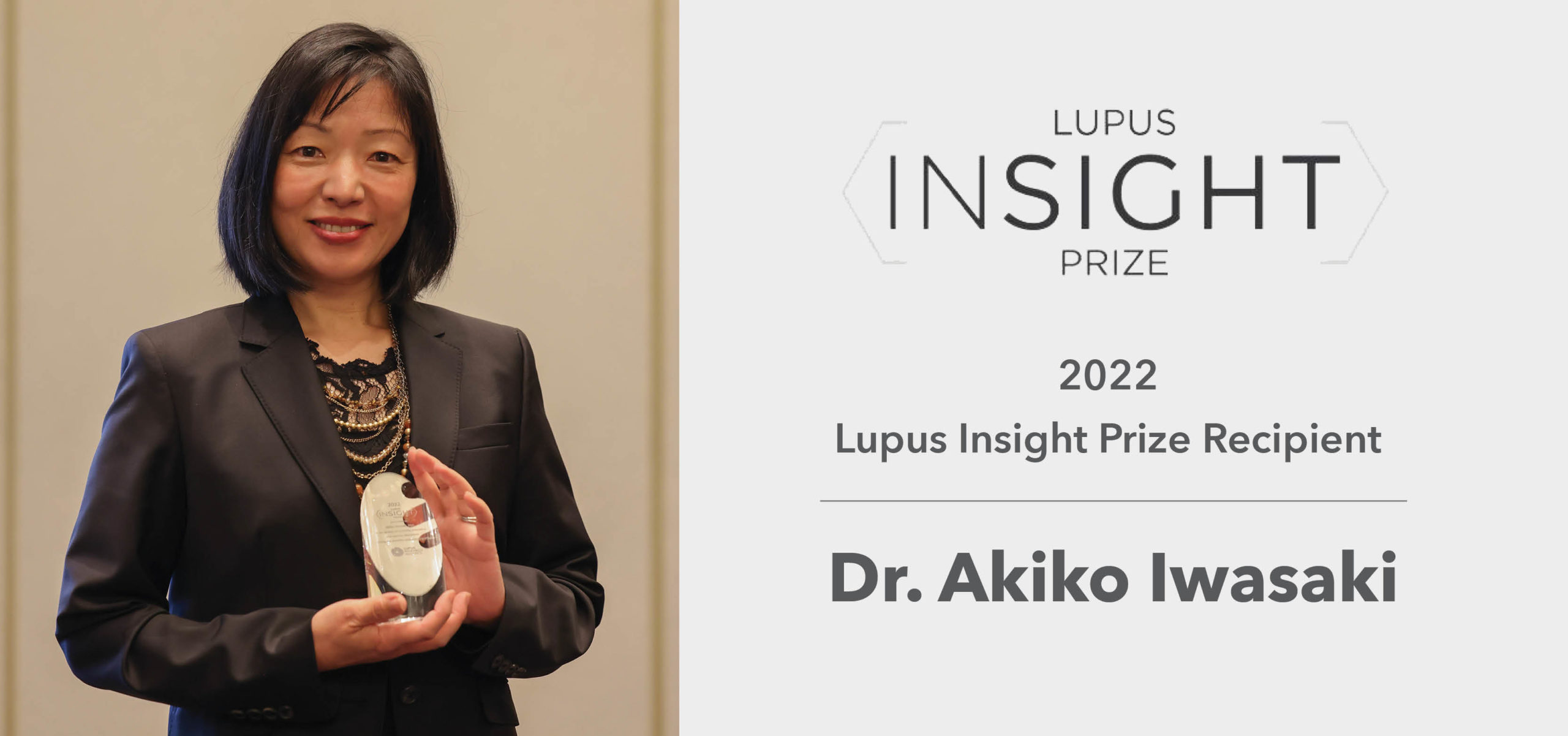
Lupus Research Alliance Awards 2022 Lupus Insight Prize to Immunologist Dr. Akiko Iwasaki: Renowned immunology expert honored
June 23, 2022
The Lupus Research Alliance (LRA) is pleased to award its 2022 Lupus Insight Prize (LIP) to Akiko Iwasaki, PhD, for her discovery of the link between endogenous retroviruses and systemic lupus erythematosus (SLE). The award was presented to Dr. Iwasaki at the 22nd Annual Meeting of the Federation of Clinical Immunology Societies (FOCIS 2022) by Judith James, MD, PhD, LRA Scientific Advisory Board member and Lou Kerr Chair in Biomedical Research and Chair of the Arthritis and Clinical Immunology Program at the Oklahoma Medical Research Foundation. The $100,000 award recognizes and honors an outstanding investigator who has, within the past five years, published a novel and important research insight into lupus that advances our understanding of this disease and could open new avenues for lupus diagnosis and treatment.
Dr. Iwasaki is the Sterling Professor of Immunobiology and Professor of Dermatology and of Molecular, Cellular, and Developmental Biology and of Epidemiology (Microbial Diseases) at Yale School of Medicine, and an Investigator at the Howard Hughes Medical Institute. Dr. Iwasaki was elected to the National Academy of Sciences in 2018, the National Academy of Medicine in 2019, the European Molecular Biology Organization in 2021, and the American Academy of Arts and Sciences in 2021.
“Dr. Iwasaki’s research shows that endogenous retroviruses are not just silent inhabitants in the human genome but rather active players able to provoke immune cells to engage in the destruction of the body’s own tissues and organs,” commented Dr. James. “This finding is highly significant because endogenous retroviruses have been increasingly associated with several chronic diseases including cancer, neurodegenerative, and autoimmune rheumatic diseases, though their exact role in human diseases remains poorly understood.”
“I am honored to receive this prestigious award, and I sincerely thank the Lupus Research Alliance for recognizing our research. I am eager to use this award to further understand the association between antibodies against the endogenous retroviruses and lupus-like disease in long COVID patients to ultimately improve their disease treatment outcomes,” said Dr. Iwasaki.
Dr. Iwasaki’s seminal discovery demonstrated that endogenous retroviruses, which are viruses that are a part of our genetic makeup or genome, make immune cells called B cells that produce autoantibodies, i.e., immune proteins that in people with SLE mistakenly target body’s own tissues, causing organ damage. Dr. Iwasaki and her team also found that endogenous retroviruses force immune cells called neutrophils to release spiderweb-like structures known as NETs, which have been shown to promote inflammation in SLE. These findings further our understanding of what may cause lupus or worsen its symptoms and suggest that targeting ways that endogenous retroviruses use to fuel inflammation in SLE could provide new therapeutic options for patients with lupus.
About Human Endogenous Retroviruses and Lupus
Human endogenous retroviruses are genetic segments of retroviral origin that have become a part of the human genetic makeup which have persisted from generation to generation and today constitute approximately eight percent of the human genome. To study the role of endogenous retroviruses in human disease, Dr. Iwasaki and colleagues initially developed the human endogenous retrovirus map, called ERVMap, which included 3,220 pieces (or segments) of different endogenous retroviruses in the human genome to be able to determine which of these genes are expressed by human cells. Among these 3,220 endogenous retroviral segments, Dr. Iwasaki’s group found that over 100 segments are strongly elevated in immune cells called peripheral blood mononuclear cells of lupus patients.
The researchers further found that these elevated levels of endogenous retroviral genes are associated with higher amounts of autoantibodies and increased type I interferon levels, which are considered a main driver of lupus. Her team also showed that the immune system of lupus patients produces autoantibodies that interact with a unique endogenous retroviral protein HERV-K102. The autoantibody HERV-K102 complexes stimulate neutrophils to release NETs, which worsens inflammation in SLE. This research was published last year in the Journal of Experimental Medicine.
About Lupus
Lupus is a chronic, complex autoimmune disease that affects millions of people worldwide. More than 90 percent of people with lupus are women; lupus is most often diagnosed during the childbearing years of 15-45. African Americans, Hispanic Americans, Asian Americans and Native Americans are two to three times at greater risk than Caucasians. In lupus, the immune system, designed to protect against infection, creates antibodies that can attack any part of the body including the kidneys, brain, heart, lungs, blood, skin, and joints.
About the Lupus Research Alliance
The Lupus Research Alliance, the largest nongovernmental, nonprofit research organization dedicated to lupus research worldwide, aims to transform treatment while advancing toward a cure by funding the most innovative lupus research in the world. The organization’s stringent peer-review grant process fosters diverse scientific talent who are driving discovery toward better diagnostics, improved treatments and ultimately a cure for lupus. Because the Lupus Research Alliance’s Board of Directors funds all administrative and fundraising costs, 100 percent of all donations goes to support lupus research programs.



