Lupus Research Alliance-Funded Researchers Present Discoveries at ACR
Lupus Research Alliance-Funded Researchers Present Discoveries at ACR
October 29, 2018
More than 70 researchers who have received funding from the Lupus Research Alliance contributed to the scientific dialogue on lupus at the ACR|ARHP meeting this year. Following are highlights of specific discoveries the organization has supported:
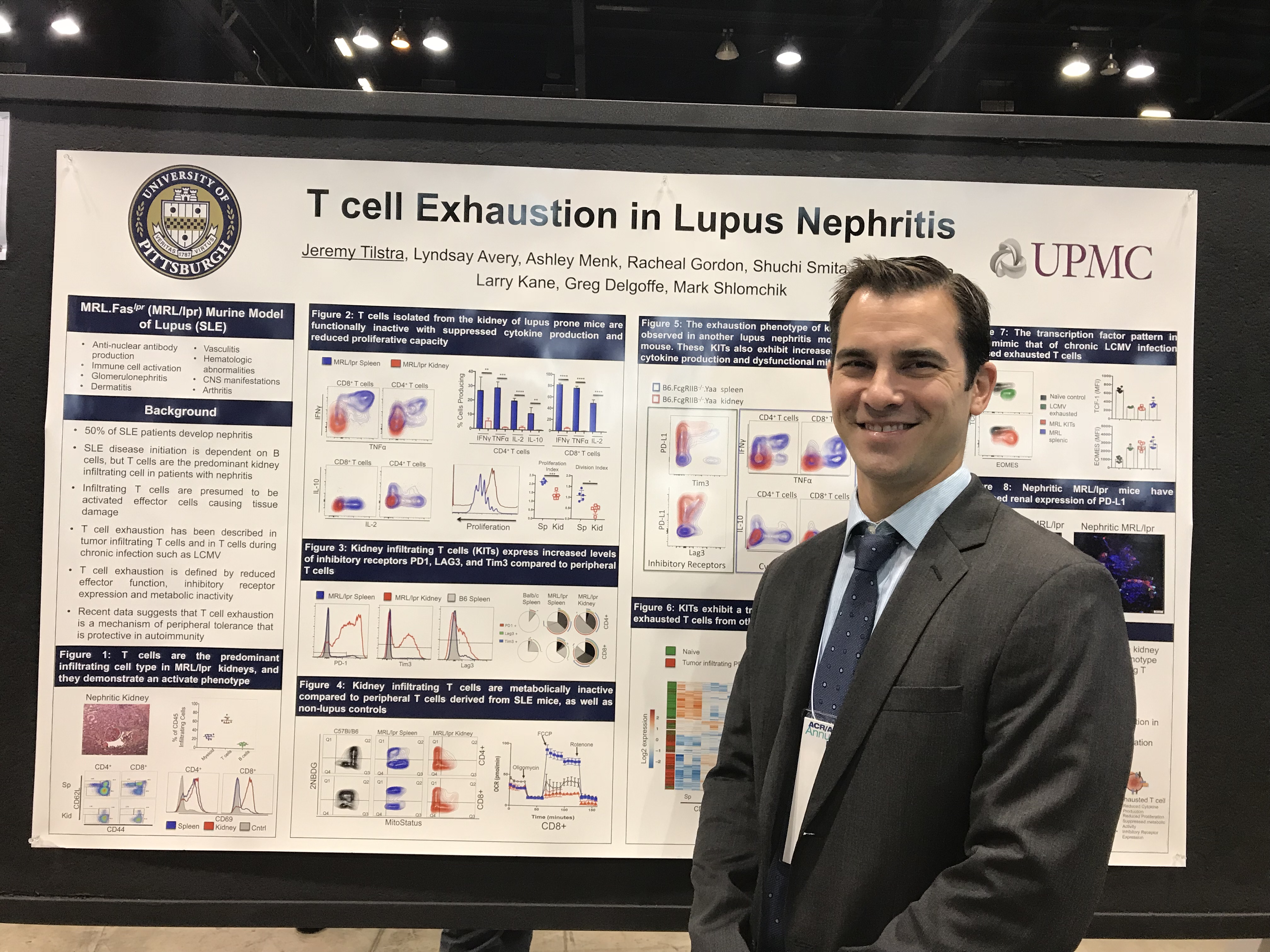
Tiring Out Rogue Cells
Learning from cancer research, a team of scientists led by the inaugural Lupus Insight Prize recipient Dr. Mark Shlomchik presented findings indicating that the kidneys may defend themselves from immune attack by exhausting kidney- infiltrating T cells. In lupus, the immune system can attack many organs, particularly the kidneys. With his 2018 Novel Research Grant from the Lupus Research Alliance, Dr. Jeremy Tilstra (first author of the abstract) aims to determine how T cells change when they enter organs commonly affected by lupus. This knowledge may enable more effective therapeutic targeting of these cells with fewer side effects.
Positive News for Potential Steroid Alternatives
The steroids that are standard lupus treatments not only cause severe side effects, but they also don’t block certain harmful molecules, known as type I interferons, that promote many of the symptoms of the disease. Two presentations (Abstracts 2092 and 2093 from Eric Morand, PhD, of Monash University in Australia and colleagues, which describe the work funded by our Distinguished Innovator Award, support the idea that targeting another molecule, known as GILZ, may overcome these problems. In mice, the researchers found, GILZ normally reduces type I interferon levels, and animals without it develop more severe lupus symptoms. The next step would be for researchers to develop a drug to stimulate GILZ or produce the same effects, which could curb levels of type I interferons and provide a new treatment for the disease.
Cleanup Enzyme Fails in Lupus Nephritis
In patients with lupus, DNA released by dead cells can trigger an abnormal reaction by the immune system. Results presented of work that was supported by the Distinguished Innovator Award to Boris Reizis, PhD, of the NYU School of Medicine suggests that an enzyme (called DNase1L3) that normally cleans up this DNA doesn’t work properly or is missing in people who have lupus nephritis, a type of kidney damage caused by the disease. The researchers discovered that blood samples from patients with lupus nephritis showed signs of an immune system reaction against DNA. Importantly, this reactivity was disrupted by treatment with the DNase1L3 enzyme. The scientists suggest that the enzyme is a possible target for lupus treatments.
Targeting the Protein that Can Worsen Lupus
A presentation at ACR of work led by Anne Davidson, MBBS, suggests that the protein TLR8 that enables immune cells to detect bacteria and viruses actually worsens lupus symptoms. Davidson and colleagues studied mice that were genetically modified to make human TLR8 and found that in certain circumstances it caused pregnancy loss and blood abnormalities such as anemia and low platelet counts. The results suggest that TLR8 is a possible target for drugs to treat some lupus symptoms that don’t involve the kidneys. This work was funded by Dr. Davidson’s Target Identification in Lupus grant from the Lupus Research Alliance.
Testing for DNA May Detect Active Disease
With his Novel Research Grant, Christian Lood, PhD, of the University of Washington in Seattle and colleagues may have discovered a new way to identify which patients with lupus have active disease. The scientists previously found that blood from mice with lupus contained DNA from mitochondria, structures within cells that provide them with energy. Now, the work they presented at ACR shows that patients with lupus have more mitochondrial DNA in their blood than people who don’t have the disease. Moreover, patients whose lupus was active carry more mitochondrial DNA than patients with inactive disease, suggesting that testing for this type of DNA could distinguish these groups of patients.