The most common symptoms of lupus are extreme fatigue, skin rashes, joint pain and unexplained fevers.
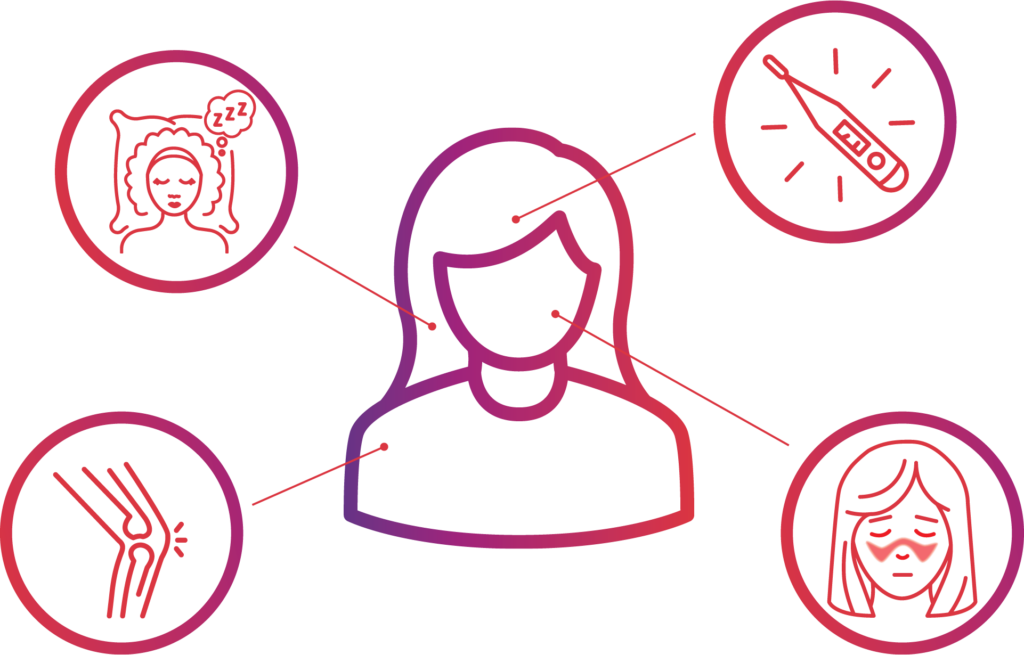
FATIGUE
Approximately 50%–90% of people with lupus identify fatigue as one of their primary symptoms. The severe fatigue of lupus seems to be caused by many factors, including disease activity, anxiety disorders, sleep disturbances, vitamin D deficiency and low levels of exercise. Scientists differ on whether there is also a relationship between fatigue and the disease itself or the treatments used to manage lupus.
No matter the cause, it’s clear that fatigue can significantly impact patients’ quality of life, including lessening the ability to function at home and at work. Research conducted through a clinical trial network established by the Lupus Research Alliance explored a potential mobile application for patients to report and measure fatigue.
MALAR RASH (BUTTERFLY RASH)

SENSITIVITY TO THE SUN
Because many people with lupus are sensitive to sunlight (called photosensitivity), skin rashes often first develop or worsen after being out in the sun. Some people find that the appearance of the butterfly rash is a sign of an oncoming disease flare.
JOINT PAIN AND SWELLING (ARTHRITIS)

FEVER
Potential Complications
Antiphospholipid antibody syndrome (APS)
Antiphospholipid antibody syndrome (APS) is an autoimmune disorder associated with lupus. Antibodies, a type of protein, help defend the body against infections, but with APS, the body makes antibodies that mistakenly attack phospholipids, a type of fat that damages cells, including blood cells. This damage causes blood clots to form in the body’s arteries and veins, which can block blood flow and damage the body’s organs.
Blood vessel inflammation
Lupus causes tissue and organ inflammation. Inflamed blood vessels (vasculitis) can affect the way blood circulates through the body. People with lupus are also at an increased risk for atherosclerosis, commonly known as hardening of the arteries.
Diabetes
Patients with lupus are at a high risk for insulin resistance and diabetes (an inability to control glucose, or blood sugar). While corticosteroids are a common treatment for lupus-related inflammation, they can interfere with insulin production. If you’re a lupus patient with diabetes, you have an increased risk for developing such complications as neuropathy (disease or dysfunction of peripheral nerves, which may cause numbness or weakness) and kidney failure.
Heart disease
For some lupus patients, inflammation can occur in the heart (myocarditis and endocarditis) or the membrane that surrounds it (pericarditis), causing chest pain or other symptoms. Endocarditis can damage the heart valves — the valve surface can thicken and develop growths. This can cause heart murmurs, though the valves can usually still function.
Kidney problems
When the kidneys become inflamed (nephritis), they can’t effectively get rid of waste products and other toxins from the body. While there is usually no pain associated with nephritis, some patients may notice dark urine and swelling around their eyes, legs, ankles or fingers. Typically, an abnormal urine or blood test is the only indication of kidney disease. But because the kidneys are so important to overall health, lupus patients with kidney disease generally require intensive drug treatment to help prevent permanent damage.
Lung problems
Some people with lupus develop pleuritis, an inflammation of the chest cavity lining. Pleuritis can cause chest pain and difficulty breathing. Patients with lupus may also be susceptible to pneumonia.
Neurological dysfunction
Lupus can affect the brain or central nervous system in some lupus patients. This is called neuropsychiatric lupus (NPSLE), and symptoms may include headaches, dizziness, depression, memory disturbances, vision problems, seizures, stroke or changes in behavior.
Pregnancy risks
Most women with mild-to-moderate lupus can have healthy babies with no complications. (It’s best to have no symptoms and take no medications for several months before becoming pregnant.) But pregnancy in women with lupus is still considered high risk. Some women may experience a mild-to-moderate flare during or after their pregnancy. Some, especially those taking corticosteroids, are more likely to develop high blood pressure, diabetes, hyperglycemia (high blood sugar) and kidney complications. If you’re pregnant and have lupus, you should seek pregnancy counseling as early as possible and see the doctor often to be monitored.
Spinal cord inflammation
Autoimmune disorders like lupus can contribute to transverse myelitis, an inflammation of the spinal cord. Transverse myelitis pain can begin suddenly in your lower back and may shoot down your legs or arms or around your chest or abdomen. Pain symptoms vary depending on the affected part of your spinal cord. Some people report sensations of numbness, tingling, coldness, burning or a weakness in their arms or legs. They also may experience problems with bowel or bladder control.




